|
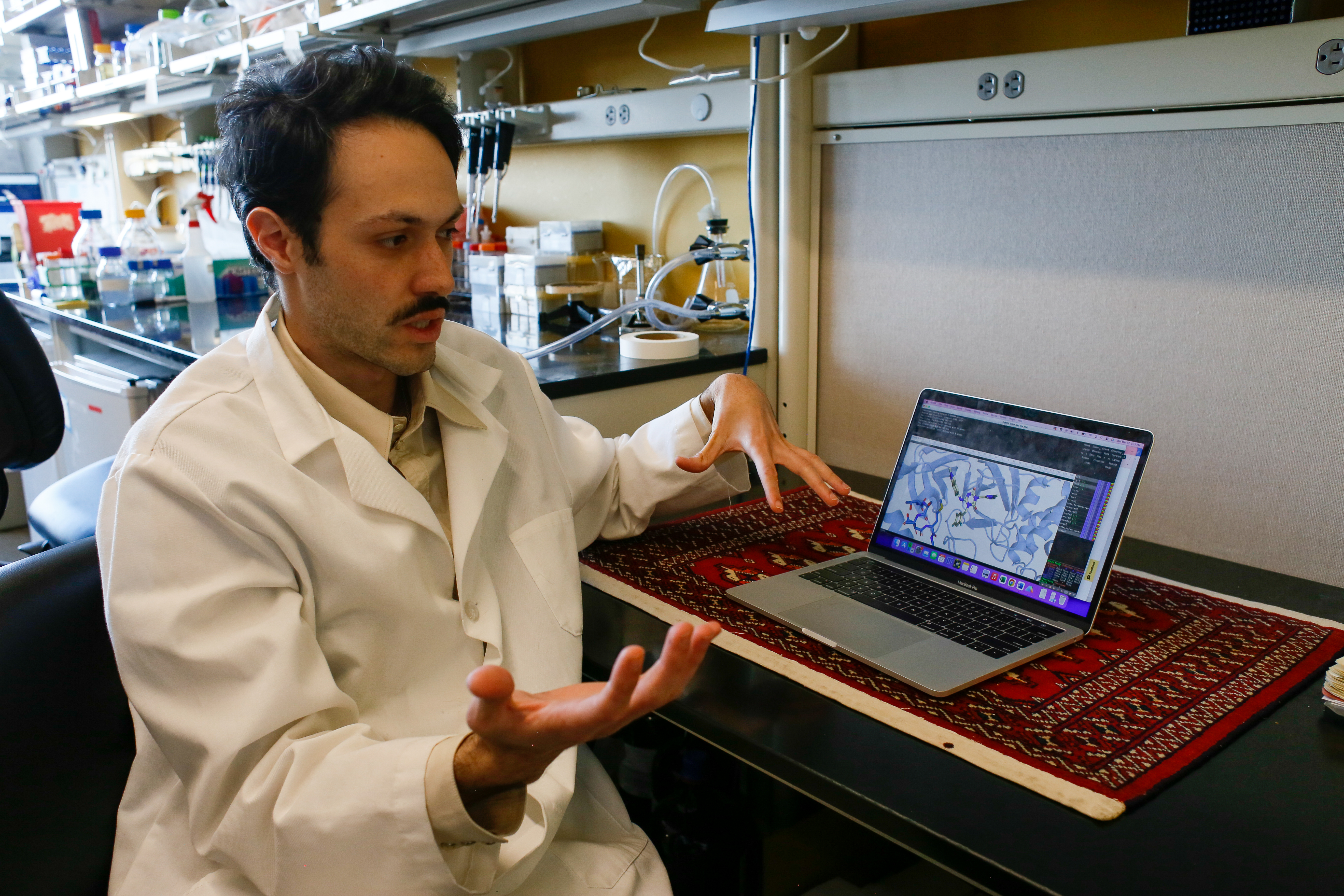
Minneapolis/St. Paul(03/29/2023) — Resistance to Paxlovid is already evident among viral SARS-CoV-2 variants currently circulating globally, indicating that this stand-alone drug known as a protease inhibitor could soon become less effective in treating COVID-19 infections. This conclusion was presented in a study published today online in the peer-reviewed journal Science Advances. This study — conducted by the Midwest Antiviral Drug Discovery (AViDD) Center — shows that drug-resistant variants have appeared multiple times independently in different parts of the world, with regional clusters providing evidence for person-to-person transmission. In addition to showing resistance to the protease inhibitor nirmatrelvir, the active component of Paxlovid, the study found that a different set of mutations currently in circulation can transfer resistance to ensitrelvir (Xocova), a protease inhibitor now approved in Japan. This new research shows that simple single amino acid changes in SARS-CoV-2 main protease could severely undermine efficacy of these antiviral drugs. According to Reuben Harris, PhD, co-director of the Midwest AViDD Center, “although our study demonstrates the existence of natural circulating SARS-CoV-2 variants with resistance to two different drugs, the good news is that their resistance profiles are distinct. This means that if one of these drugs fails due to emergence of resistance in viral variants, the other drug may still work.” Further research is likely to develop additional next-generation protease inhibitors with different resistance profiles, as well as drugs that target different viral processes such as replication or cell entry. A multi-drug approach—like existing therapies for HIV and Hepatitis C virus — could further help to protect against resistance and cure SARS-CoV-2-infected individuals. To lower the risk of resistance, the researchers say protease inhibitors must be carefully designed to avoid simple resistance mutations. “Despite Paxlovid’s proven success in blunting COVID-19 symptoms, the long-term consequences of its widespread use in speeding up resistance are unknown,” said S. Arad Moghadasi, co-author of the study and a University of Minnesota Medical School graduate student. “Drugs with the highest barriers to resistance are likely to prove more effective and have longer-term durability.” “We are optimistic that ongoing studies will develop additional compounds to avoid cross-resistance and help combat the current COVID-19 pandemic and future coronavirus outbreaks,” said Harris, a professor and chair of biochemistry and structural biology at the University of Texas Health Science Center at San Antonio, a Midwest AViDD Center partner, and an investigator of the Howard Hughes Medical Institute. This research was supported by the National Institute of Allergy and Infectious Diseases (U19-AI171954). ### About the Midwest AViDD Center The Midwest AViDD Center is developing the next generation of antiviral drugs for pandemic-level viruses, including SARS-CoV-2, Ebola, Lassa, and Zika. Headquartered at the University of Minnesota and including 18 other institutions nationwide, the Midwest AViDD Center is part of a network of nine national centers established by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health.
For media requests, please contact: Kali Kotoski, Communications Director for the Midwest AViDD Center 651-338-0619, [email protected] |